Understanding Health Disparities
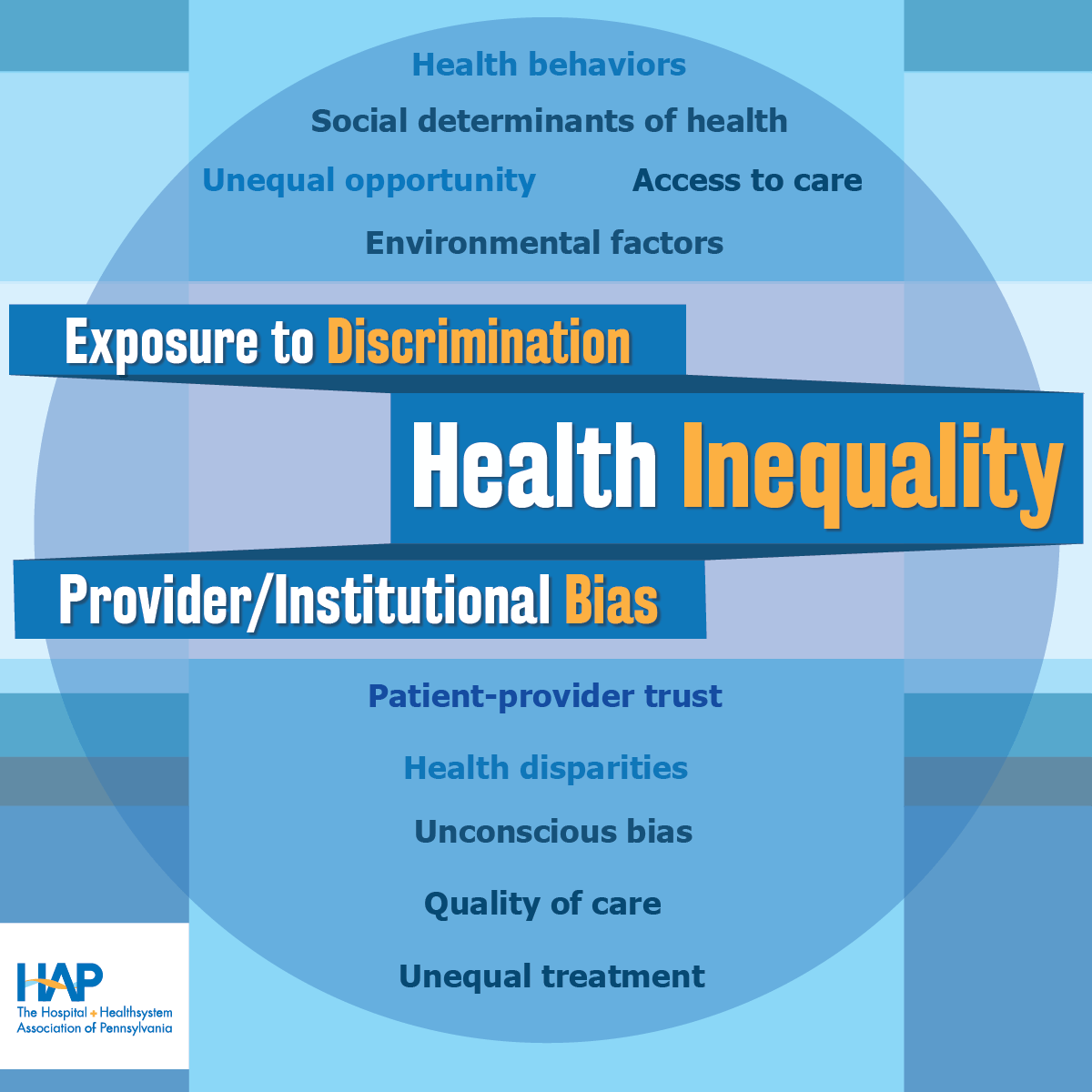 Evidence overwhelmingly points to bias and racism as the root cause of health inequity in the U.S. Across many measures, health outcomes are often worse for communities that have been marginalized and discriminated against on the basis of race, ethnicity, sex, nationality, language, sexual orientation, gender identity, disability, and other factors.
Evidence overwhelmingly points to bias and racism as the root cause of health inequity in the U.S. Across many measures, health outcomes are often worse for communities that have been marginalized and discriminated against on the basis of race, ethnicity, sex, nationality, language, sexual orientation, gender identity, disability, and other factors.
For example:
- The CDC notes that racial and ethnic minority populations, compared with white populations, experience higher rates of diabetes, hypertension, obesity, asthma, and heart disease and that the life expectancy for Black Americans is four years lowers than that of white Americans.
- A 2021 study of 30 U.S. cities from 2016–2018 estimated that health inequities contribute to 74,402 more deaths annually among Black people than white people.
- Pennsylvania’s 2022 state health assessment found that the maternal mortality rate in the commonwealth from 2015–2019 was more than twice as high for Black people as it was for white people.
- In a 2021 survey of LGBTQ youth, 42 percent reported seriously considered attempting suicide and 48 percent reported that they wanted counseling from a mental health professional but were unable to obtain it.
Eliminating these inequities—and the racism and biases that cause them—is central to promoting health equity.